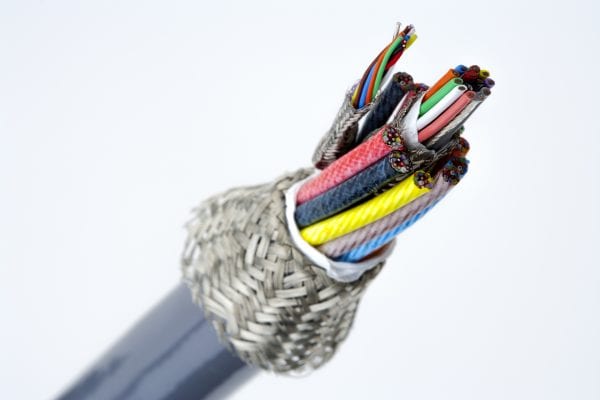
Biocompatibility is ultimately a function of a completed device including all of its components, assembly processes and overall design. However, thoughtful material selection will help contribute to a product’s overall biocompatibility.
When design engineers speak of biocompatibility they are referring to how a device interacts with bodily tissues. The goal of biocompatibility is to prevent damage to organs and cells. The material used to make the cable jacket should prevent toxic damage.
For example, if a cable jacket will come in contact with tissues, the length of time it is in contact without doing damage—that is, without toxicity—is important. A device with only limited contact can meet less stringent specifications than one to be implanted. Likewise, an implantation can be defined as short term (less than 24 hours), prolonged (24 hours to 30 days) or permanent (more than 30 days). Each duration interval can affect the kind of cable jacket material chosen to assure biocompatibility. Moreover, choosing the best biocompatible jacket depends on which body part is at issue. Contact with skin, mucosal membrane, blood, bone and other body parts may each require different jacket materials.
Biocompatibility Standards and Testing
Testing for biocompatibility is a systematic process that aims to evaluate a medical device’s biological safety so that risk damage to the human body can be prevented. Such testing can be difficult, time-consuming and costly. Medical device designers have been aided by guidelines that specify what to look for and how to test.
The Tripartite Biocompatibility Guidance for Medical Devices was released to the U.S., the U.K. and Canada by the U.S. Department of Health and Human Services in 1986. It served as a handbook for determining the toxicity of medical devices and their components. The original distribution of the handbook was accompanied by a memo that said “it would be circulated … for comment and use ‘as appropriate.'”
The handbook didn’t guarantee medical devices built to its specifications would pass the Office of Device Evaluation’s inspection, but it offered clear guidance to medical device manufacturers and was widely used until 1995. Then, the U.S. FDA produced its own version of the International Organization for Standardization’s ISO 10993. It came to be known as ISO 10993-1, and has since been used to make design decisions for new medical device. The FDA standard includes a table that defines devices by contact type and duration as mentioned above. Tests for biological response are then specified according to the resulting category. The standard is intended to offer guidance rather than an exclusive checklist for qualification of new medical devices.
At present, European medical electronics manufacturers use the original ISO 10993 standard. However, U.S. manufacturers refer to the FDA’s ISO 10993-1 edition, while Japan follows its “Japanese Guidelines for Basic Biological Tests of Medical Materials and Devices” along with the original ISO standard. This diversity of standards, even though overlapping in some areas, complicates medical device design for a worldwide market.
The ISO standard provides advice on topics such as…
-Guidance on the selection of tests to be used
-Animal welfare requirements
-Testing for genotoxicity, carcinogenicity, and reproductive toxicity
-Selection of tests to identify interactions with blood
-Tests for cytotoxicity—in vitro methods
-Tests for local effects after implantation
-Ethylene oxide sterilization residuals
-Degradation of materials related to biological testing
-Tests for irritation and sensitization
-Tests for systemic toxicity
-Sample preparation and reference materials, and more.
Beyond Biocompatibility
In addition to biocompatibility, other issues require attention in selecting cable jacket material. For example, sterilization methods can degrade jacket material. Therefore, design engineers should consider the kind of sterilization protocols to be used early in the design process, then reconfirmed them as the product moves through prototype and qualification steps.
Sterilization technologies include gamma radiation, ethylene oxide, autoclave with increasingly higher temperatures, peroxide plasma systems and others. Cable jackets must meet biocompatibility and environmental regulatory expectations, and must also maintain those characteristics after repeated sterilization. The ability of any material to endure sterilization processing is a function of polymer type and grade, crystallinity, molded stresses thickness and even packaging. Furthermore, each sterilization process itself includes variables that may affect material stability.
Radiation sterilization, for instance, involves a dosage range somewhere between the minimum necessary to achieve a sterility assurance level (SAL) and maximum acceptable dose for device and material function. Radiation source selection (e-beam, gamma or x-ray) will affect depth of penetration.
Packaging is significant in radiation sterilization as well. Variations in type, orientation and bulk density will change the radiation dosage to various parts of the device(s) within the chamber. Just as radiation sterilizes by disrupting molecular bonds, cable jacket polymers may be disrupted by undergoing either chain scission or cross linking. Either result can have undesirable effects such as embrittlement, softening and discoloration.
Polyacetal, polypropylene, and PTFE are especially susceptible to radiation degradation. Certain materials can be compounded with stabilizers to minimize the effects of radiation (e.g., PVC). Radiation techniques have a long history of effectively sterilizing devices with intricate designs and inaccessible surfaces. Devices are ready for use immediately upon completion of the cycle, without chemical residues. The limitation is in the polymer response to the source, dose and other exposure variables.
Ethylene oxide (EO) sterilization presents a number of variables to consider during cable jacket selection. EO conditions such as temperature, pressure changes, humidity, EO concentration and exposure time are optimized for device design through a validation process. Following sterilization, residual EO must be removed through a heated aeration process. This process is often the limiting factor in material selection.
Devices intended to be steam (autoclave) sterilized must consider temperature, humidity, pressure and repeated cycling. Materials with low tolerance for heat and steam may soften, melt, discolor or react. Poorly bonded or sealed parts may provide an opportunity for steam to penetrate to conductors or other metal parts. Corrosion may be initially undetected, yet lead to costly failures in the field.
Hydrogen peroxide systems, using either vapor or plasma sterilization, can be used with materials that do not tolerate high temperatures and humidity, and with corrosion-susceptible metal alloys. Unlike EO sterilization, hydrogen peroxide systems do not need a heated aeration process. Peroxide sterilizers generally complete a cycle in an hour or less which, of itself, places lower stress on cable jackets than other methods.
Conclusion
New England Wire Technologies has long focused on biocompatibility. We have studied and tested a large number of jacket materials for irritation, sensitivity and cytotoxicity. Our engineers are knowledgeable on a wide range of thermoplastics, thermosets, coatings, sterilization techniques, caveats, modes of failure, and related topics that lead to more reliable medical device products.
Biocompatibility requirements are specific to each device type (surface, external communicating, implant) and contact duration (limited, prolonged, or permanent). Contact us to discuss biocompatibility issues and any sterilization questions you may have. We’re happy to help you select cable jacket material and, thereby, shorten the qualification process by avoiding over specifications or choosing inadequate materials.